(D.R.S.A.) Airway
To Check Airway:
Open the mouth gently without moving the head or the neck at this early stage in case there have been any injuries to the spinal cord.
Airway Management
When a casualty becomes unconscious their muscles including the tongue and the soft tissue of their throat relax. Particularly if a casualty is lying on their back, this relaxed tongue falls back and blocks the airway preventing air from reaching the lungs.
Airway obstruction in an unconscious casualty can be caused by the tongue becoming relaxed and falling backwards and foreign material such as vomit, food or blood. The casualty is unable to swallow or cough out the foreign material and to prevent obstruction all foreign material must be removed. The only way a first aider can remove any obstruction at the back of the throat is to roll the casualty onto their side using what is called a hip and shoulder roll. Special care should be taken if there is a risk of spinal cord damage.

including a suspected spinal injury.
(D.R.S.A.B.) Breathing
Checking for Breathing
After an unconscious casualty’s airway has been assessed as clear, use the look, listen and feel technique to check for normal breathing. This step should not be rushed as you might miss the signs, take at least 15-20 seconds, and if breathing is NORMAL you should see between 4-5 rises and falls of the chest in that time.
Put your cheek near the casualty’s mouth and nose. Look down and along the chest and
- Look – for the rise and fall of the chest.
- Listen – for any sound, and any breathing.
- Feel – for the movement of air from the nose and mouth against your cheek, and place your hand on the casualty’s chest to feel for the rise and fall.
In the first few minutes of a casualty’s cardiac arrest, sounds of gurgling, sighing or coughing may be present, as well as movements of the chest and stomach. This type of breathing is ineffective, as it does not move air into or out of the lungs and the casualty should be treated as if they are not breathing.
Breathing may be absent or ineffective as a result of:
 Brain damage.
Brain damage. Upper airway obstruction.
Upper airway obstruction. Paralysis or impairment of nerves and/or muscles of breathing.
Paralysis or impairment of nerves and/or muscles of breathing. Respiratory problems.
Respiratory problems. Immersion.
Immersion. Cardiac arrest.
Cardiac arrest.If you are not sure if a casualty is breathing normally, treat as if they are not breathing.
(D.R.S.A.B.C.) Compressions
Cardiopulmonary Resuscitation (CPR) is the technique of compressing the chest to move oxygenated blood around the casualty’s body and inflating the lungs with your breath to provide a supply of oxygen to the casualty. Without oxygen being delivered to the body’s cells they will begin to die within 3 to 5 minutes and by 7 to 11 minutes without oxygen, the brain is damaged past the point of repair. These simple techniques will either restart normal heart/lung action or maintain circulation sufficient to preserve brain function until medical assistance arrives.
The two main components of conventional CPR are chest compressions to make the heart pump and mouth-to-mouth ventilation to breathe for the casualty. Hands-only CPR is a form of resuscitation that involves continuous, rapid chest compressions only, and although effective, if not done correctly it is not as beneficial.
Commence CPR if the signs of breathing are abnormal.
CPR requires the first aider to give 30 compressions followed by 2 breaths (1 cycle).
Chest Compressions
Compressions are performed with the casualty laying on a firm surface; the floor is suitable for an adult. In the case of a small infant, compressions are best performed on a table or similar surface. This will ensure the resuscitator is as comfortable as possible and can continue until medical assistance arrives.
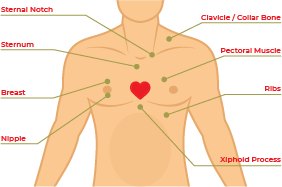
Locate the “centre” of the chest – this is the lower bottom half of the sternum
.
Adult, Children and Infants
1 Kneeling beside the casualty with one knee level with the chest and the other knee level with the head.
2 Locate the lower half of the sternum in the centre of the chest.
3 Place the heel of one hand on the lower half of the sternum (breastbone) and place the heel of the other hand on top of the first hand, interlock fingers of both hands and raise fingers to ensure that pressure is not applied over casualty’s ribs, upper abdomen or bottom part of the sternum.
4 Position yourself vertically above the casualty’s chest.
5 With straight arms, press down on the sternum (breastbone) to depress approximately one-third of the depth of the chest. Compressions should be given at a rate of almost 2 per second. You should achieve 5/6 cycles of 30 compressions and 2 breaths in 2 minutes.
6 Repeat to complete 30 compressions at a rate of approximately 100/120 per minute.
Special Considerations in CPR
Pregnant Casualty
A woman in advanced stage of pregnancy (20+ weeks) requiring CPR should be positioned on her back with shoulders flat on the ground. Place padding under her right buttock to tilt the pelvis to the left. This takes the baby off the main blood supply back to the heart (the Inferior Vena Cava). If padding is not available to achieve a definite tilt, a second person should gently tilt the hips to the left side while CPR is being performed.
Rescue Breathing
On breathing in, a person inspires approximately 21% oxygen, and the body uses between 4-5% of this amount for its normal functions. Therefore, when a person breathes out (expiration) they expire approximately 16% of oxygen.
If an unconscious casualty is not breathing normally after the airway has been opened and cleared, compressions must be given at a rate of nearly 2 per second. If there is still no signs of response begin rescue breathing. Rescue breathing is when the first aider delivers air/oxygen into the mouth of the casualty (mouth-to-mouth resuscitation). It is an effective way to provide oxygen to a non-breathing casualty.
![]() Place one hand on the casualty’s forehead or top of the head.
Place one hand on the casualty’s forehead or top of the head.
![]() With the other hand place your thumb over the chin below the lip and support the tip of the jaw with the knuckle of the middle finger. The hand is held in a pistol grip fashion with the index finger lying along the jawline. Be careful to prevent the ring finger from squashing the soft tissues of the throat as this may block the airway.
With the other hand place your thumb over the chin below the lip and support the tip of the jaw with the knuckle of the middle finger. The hand is held in a pistol grip fashion with the index finger lying along the jawline. Be careful to prevent the ring finger from squashing the soft tissues of the throat as this may block the airway.
![]() In children one to eight years of age, the head should only be given a half tilt backwards.
In children one to eight years of age, the head should only be given a half tilt backwards.
![]() In infants, younger than one year of age, the head should be kept in a neutral position. DO NOT tilt the head.
In infants, younger than one year of age, the head should be kept in a neutral position. DO NOT tilt the head.
![]() Gently pull the casualty’s jaw up towards you using a pistol grip, as you are extending the jaw slide the head back into a tilt. The head is tilted backwards, NOT the neck.
Gently pull the casualty’s jaw up towards you using a pistol grip, as you are extending the jaw slide the head back into a tilt. The head is tilted backwards, NOT the neck.
![]() Seal their mouth with yours, blow until you see a rise of the casualty’s chest indicating movement of air to the lungs
Seal their mouth with yours, blow until you see a rise of the casualty’s chest indicating movement of air to the lungs
![]() By combining correct head tilt and effective chin lift, you open and clear the airway and reduce the risk of regurgitation.
By combining correct head tilt and effective chin lift, you open and clear the airway and reduce the risk of regurgitation.
There are three types of head tilt used in resuscitation:
- Neutral – used for infants (0-1 years) and casualties who have a suspected spinal injury.
- Half tilt – used for young children (1-8 years).
- Backward – used for older children and adults (8 years and upwards).
Rescue Breathing Techniques
Using the Mouth-to-Mouth Rescue Breathing method.
The first aider seals the casualty’s mouth with their own mouth, and then blows air into the casualty’s mouth pinches the nose closed if air leaks from the nose.
Mouth-to-Nose Rescue Breathing
This technique is used when the casualty has sustained facial injuries such as broken teeth or jaw, the jaw is tightly clenched or resuscitation is performed in deep water.
Mouth-to-Mask Rescue Breathing
This technique requires a resuscitation mask (CPR face shield). It prevents mouth-to-mouth contact between the first aider and the casualty. This technique is recommended if the casualty has vomited, there is blood present, the casualty is intoxicated or unknown to you. The mask is fitted firmly over the casualty’s mouth and nose and the first aider delivers breaths via a valve or tube that prevents direct contact with the casualty’s skin or expired air.

- Infant – Less than 1 year of age.
- Child – Between 1 to 8 years of age.
- Adults – 8 years of age and older.

Only deliver enough breath to a casualty to make their chest rise.
![]() Place them on their side in the recovery position and maintain neck stability.
Place them on their side in the recovery position and maintain neck stability.
![]() Re-check the casualty’s airway and breathing regularly.
Re-check the casualty’s airway and breathing regularly.
![]() Check for other injuries. Identify and immediately control any severe bleeding. This simply requires the casualty to be scanned from head to toe to detect signs of external bleeding. Bleeding is considered severe when it is spurting or cannot be controlled. Such severe bleeding is a life-threatening condition that must be addressed as quickly as possible.
Check for other injuries. Identify and immediately control any severe bleeding. This simply requires the casualty to be scanned from head to toe to detect signs of external bleeding. Bleeding is considered severe when it is spurting or cannot be controlled. Such severe bleeding is a life-threatening condition that must be addressed as quickly as possible.
(D.R.S.A.B.C.D) Defibrillation
Attach an Automated External Defibrillator if available and follow the voice prompts.
An AED is an electronic device that automatically analyses the casualty’s heart rhythm, an AED will not shock if the heart has completely stopped (Cardiac arrest). If it detects a problem that may respond to an electrical shock, it permits a shock to be delivered in an attempt to restore a normal heart rhythm.
![]() Send someone for the AED.
Send someone for the AED.
![]() If there is more than one first aider present, assign tasks for each.
If there is more than one first aider present, assign tasks for each.
![]() Turn on the AED.
Turn on the AED.
![]() Attach the electrode pads. If there is another first aider, continue chest compressions while the pads are attached.
Attach the electrode pads. If there is another first aider, continue chest compressions while the pads are attached.
![]() Follow the voice/visual prompts of the AED.
Follow the voice/visual prompts of the AED.
![]() Ensure that nobody touches the casualty while the AED is analysing the rhythm.
Ensure that nobody touches the casualty while the AED is analysing the rhythm.
Pad Placement for Adults
Place pads on the exposed chest with 1 pad near the top of the right side of the chest and the other below the left bottom of the chest, the pads will have a diagram to sure you where to position, if placed in the wrong place the AED will advise you. “Adjust Pads-Adjust Pads” until you have found the correct position. In large-breasted individuals it is reasonable to place the left electrode underneath the left breast, avoiding breast tissue. All pads have a diagram on the outer covering demonstrating the area suitable for pad placement.
Pad to skin contact is important for successful defibrillation. There may be a need to remove moisture or excessive chest hair prior to the application of pads but emphasis must be on minimizing delays in shock delivery.
Avoid placing pads over implantable devices. If there is an implantable medical device the defibrillator pad should be placed at least 8 cm from the device. Do not place AED electrode pads directly on top of a medication patch because the patch may block the delivery of energy from the electrode pad to the heart and may cause small burns to the skin. Remove medication patches and wipe the area before attaching the electrode pad.
Pad Placement for Children
Standard adult AEDs and pads are suitable for use in children older than 8 years. Ideally, for children between 1 and 8 years paediatric pads and an AED with a paediatric capability should be used. These pads also are placed as per the adult and the pads come with a diagram of where on the chest they should be placed.
If a Shock is Indicated
- Ensure that nobody touches the casualty.
- Push the shock button as directed.
- Continue to follow the voice/visual prompts of the AED.
If No Shock is Indicated
- Immediately resume CPR.
- Continue to follow the voice/visual prompts of the AED.
AED Safety
The precaution and proper use of an AED are very important to ensure it operates effectively and prevents injury.
The AED operator is responsible for using the AED in a safe manner.
First Aiders and Bystanders
Keep your hands off the casualty while the AED is analysing and performing defibrillation:
- Touching the casualty while the AED performs analysis may result in an inaccurate reading.
- Touching the casualty during defibrillation may result in you or others receiving an electric shock.
-Clearly and loudly state “don’t touch the casualty” or “stand clear”.
-Look to ensure that no one is touching the casualty before pressing the shock button.
Transport
The AED device should be used with great care if the casualty is being transported. The movement of a vehicle may affect the ability of the AED to analyse the casualty and consequently affect its performance.
Surgical Implants
If a casualty has an electronic pacemaker or cardioverter implanted under the skin, ensure that the AED chest pad is positioned at least 10 cm away from the pacemaker.
Ensure that the pads are not placed over a Glyceryl Trinitrate patch (GTN).
Beware of Moisture
Before performing the defibrillation, make sure the chest of the patient is completely dry. In the AED kit you will find a cloth that is provided for the purpose of drying the casualty’s chest. Sweat or water spots make certain parts of the chest less resistant and the defibrillation might not be very effective. Also, the presence of water may lead to burns. Make sure that the casualty has no contact with water. If the casualty is in a pool or outside in wet weather remove them to a safe shelter and dry the chest before taking any further action.
DO NOT use alcohol wipes to dry the chest of the casualty as it is very flammable.
Gaseous and Oxygen-Rich Environments
Defibrillators can cause sparks. If using oxygen to supplement resuscitation, ensure that there is no concentration of oxygen around the casualty’s chest. Ensure that there is no buildup of other gases around the scene.
Signs of Life
If the casualty shows Signs of Life, roll them onto their side, treat any other injuries and continue to monitor their airway, breathing and circulation until the ambulance arrives. If the casualty is breathing and unconscious place on their side in the recovery position, check for and manage any other injuries until the ambulance arrives.


